Pediatric Brachial
Plexus Injuries
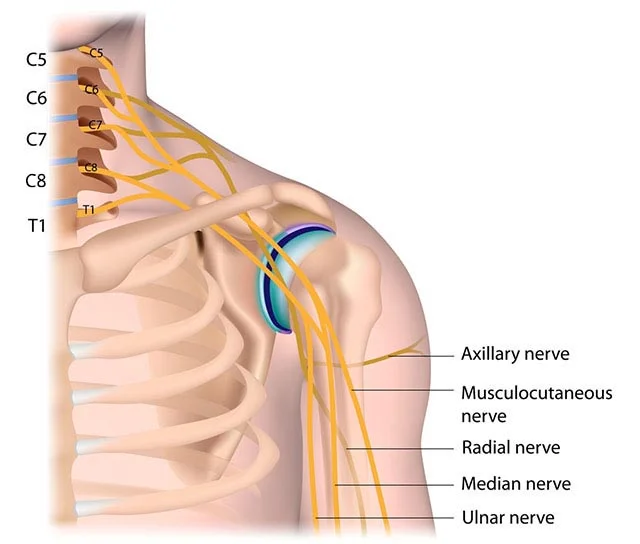
Types of Brachial Plexus Injuries
Causes of Pedriatric Brachial Plexus Injuries
Over 90% of Brachial Plexus injuries of infants are caused by trauma during birth, which is called Birth Palsy or Erb’s Palsy, depending on the involvement of certain nerves in an injury.
A small percentage of Brachial Plexus injuries are caused by other trauma rather than trauma during birth. A fall, car accident, or any other dramatic force that pulls a child’s neck and shoulder apart could cause nerve injuries.
Brachial Plexus deficits are not only caused by a child’s birth injury but are also a disease called Parsonage-Turner syndrome. Young men (including teenagers) are at higher risk of getting this disease than any other age or gender. In rare cases, a disorder called Brachial Neuritis can cause Brachial Plexus. Brachial Neuritis can be preceded by Varicella-Zoster Infection (cause of Chickenpox and Herpes.)
Brachial Plexus injuries occur roughly 2 times every 1000 births. Birth Palsy has traditionally been grouped into three categories.
Full Spectrum of Therapeutic Intervention
Getting to know you and your child is most important to us!
Our comprehensive evaluation includes:
- Assessment of function
- Collaborative goal setting
- Use of interpreter services
- Support services
- Telehealth
The most advanced therapy intervention program in the nation
- Individualized
- Stretching/Strengthening Program
- Custom Splinting
- Neuromuscular Electrical Stimulation
- Therapeutic Taping
- Serial Casting
- Modified Constraint Induced Movement Therapy
- Aquatic Therapy
- Robotic & Virtual Technology
- In-home therapy in Manhattan, Westchester and Connecticut

Personalized treatment for your child
Therapy
Therapy is essential in every child with a brachial plexus injury. Brachial plexus injuries are injuries to nerves. While therapy doesn’t directly address the nerve injury, it addresses brain development, muscle weakness & tightness, joint stiffness and contractures. Many children will recover nerve function that resulted in the brachial plexus injury but if the other areas are neglected (muscle, joint, & brain development) their final outcome will be negatively impacted. The importance of therapy for these children can not be overstated.
In many patients with Erb’s palsy, a mild paradoxical elbow flexion contracture often develops. To date, there is no definitive explanation of when and why this occurs.
Surgery
Fortunately, most children will not need surgery. But while no parent wants surgery for their child, some kids will benefit immensely from surgery. The purpose of surgery is to allow the children to achieve levels of function much better than they could have without surgery. The role and type of surgery for kids can be divided into two main groups: Nerve and Muscle/Joint.
Nerve
Regaining at least some nerve function is a realistic goal in the first ~18 months of life. As length of time from the injury (birth) increases, the degree of recovery that can be expected decreases. Therefore, if the rate of nerve recovery is too slow then we recommend surgery to address the nerve injury directly. There is a wide variety of surgical options that include neurolysis, nerve grafting, nerve transfers and various combinations of these procedures. The goal for any surgery on the nerves is to improve the communication between the brain and the ‘end organs’ (e.g. hand, muscles, sensory receptors…etc). Of course, brachial plexus injuries are a disruption of the nerves connecting the brain to these end organs. While surgery can not fully reverse the nerve injury, it has the potential of significantly improving the function of the nerves. While some nerve surgeries can allow for near perfect function other nerve surgeries allow for only small improvements. The quality of the surgery and the surgical plan have a tremendous impact on the outcome of the surgery. But the severity of the injury and the time to surgery are hugely important in how successful surgery can be. Therefore, it is critical that babies with arms that don’t seem to be moving normally or are held in slightly odd manner are evaluated for a brachial plexus injury as soon as possible and referred to a specialist by 3 months of age.
How do you determine whether my baby needs nerve surgery or not?
It is widely agreed upon that if a baby does not regain meaningful elbow flexion or biceps function by around 6 months of age that they will ultimately do best with the addition of a good surgical plan to directly address the nerve injury.
What if my child is evaluated much later than 3 months of age? Is it too late to have nerve surgery if my child is older than 1 year?
Surgery earlier is always better and the options for nerve surgery do decrease with time. However, there are still some nerve surgery options that remain. Regardless of any real or perceived delay, have your child evaluated by a specialist as soon as you can. Adult patients with birth-related brachial plexus injuries can still benefit from certain types of nerve surgeries.
Muscle / Joint
Allowing for normal growth and development of the muscles, ligaments and bones is of critical importance and the focus from very early on. Similar to the nerve injury, patients benefit most if this is addressed from a very young age. As the child grows the focus of surgery becomes more to re-balance the muscles and maintain good joint motion. Most brachial plexus injuries affect the C5 and C6 nerve roots. What this means for the child is that they have difficulties with shoulder and elbow motion. When necessary, surgery is meant to complement therapy to maintain full motion of the shoulder and the elbow. This prevents the development of contractures and abnormalities of the joints. At a young age, releasing muscles which are over-tightened is a common focus. This is commonly done through botox injections and also muscle-lengthening surgeries. Botox is temporary so gives the therapists a chance to work on aggressive stretching. Botox also has the benefit of aiding with “co-contraction”. This is where two muscle groups that are antagonistic (e.g. biceps and triceps) are both inappropriately contracting when the child attempts to perform a specific function. In the case of co-contraction of the biceps and triceps, this occurs when the child attempts to flex the elbow. The temporary and selective relaxation of one group of muscles allows the other group to strengthen and improve their overall function.
As the child grows up, tendon transfers and bony procedures can be done to allow for the arm to move as normally as possible and also have a more normal resting posture and appearance. If the degree of nerve injury is more extensive and involves the nerves that go to the wrist and hand then other surgeries can be helpful.
What is Brachial Plexus Reconstructive Surgery
How do we determine whether you need surgery or not
Depending on the severity of the injury sustained, different types of individualized treatments are offered. Brachial Plexus reconstructive surgery is necessary when therapeutic intervention and neurological recovery falters, shoulder subluxation or dislocation occurs, or contracture becomes fixed.|
Surgical decision making is a team approach with input from the medical team, the caregivers, and of course the patient to determine the best approach.
How many surgeries will my child need?
While most children will never need a surgery, some children do benefit significantly with surgical intervention. Each child and each injury are unique so we intentionally don’t try to predict how many surgeries will be most useful to give your child his or her best possible function. As your child grows up, it is necessary that all treatment decisions are made in a way to build off of the gains that the child has already made.
Day of surgery
Depending on the severity of the injury and your child’s needs, preparation for surgery and the duration of surgery varies. Our team will communicate with you prior to surgery so you know what to expect.
Prior to the surgery, child life specialists will engage with your child to make them feel at ease in a new and sometimes overwhelming environment.
Recovery
Following surgery your child may need to spend time in the hospital. Depending on the type of surgery, your child’s arm may need to be immobilized in a cast. If nerve repair is needed, it can take many months to see improvement in your child’s function as it takes time for nerves to grow. It is important to return to occupational therapy following all types of surgery, and our team will guide you through the process.
“These injuries are very complex and patients require a thoughtful and sophisticated plan for their treatment.”
Dr. Andrew Price
Make an appointment with us
(An in-house or a video visit)
212-598-2391
Monday Through Friday
9:00AM to 5:00PM (except holidays)
Ask us about your Brachial Plexus
Condition
We are here to help you plan you Brachial Plexus treatments
Share your Brachial Plexus story
with the community
Your story can inspire or help others
with Brachial Plexus injury.